CASE AT A GLANCE
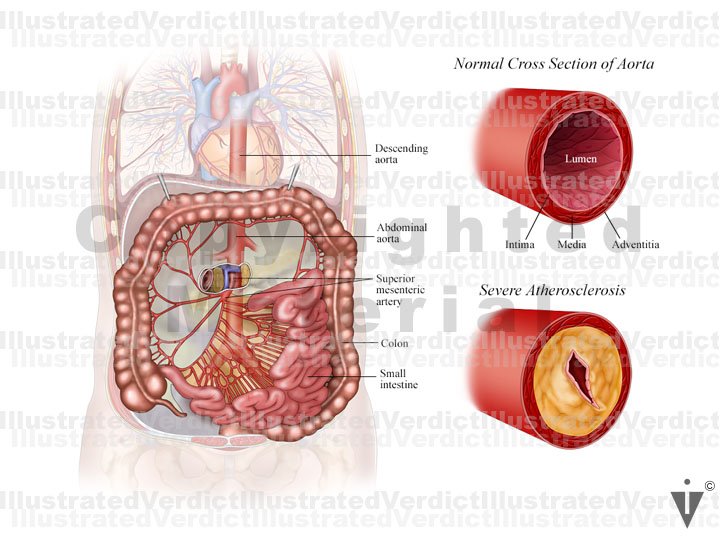
Subtotal Colectomy / Aortic Atherosclerosis
Illustrated Verdict, Inc. © All rights reserved.
Case Overview:
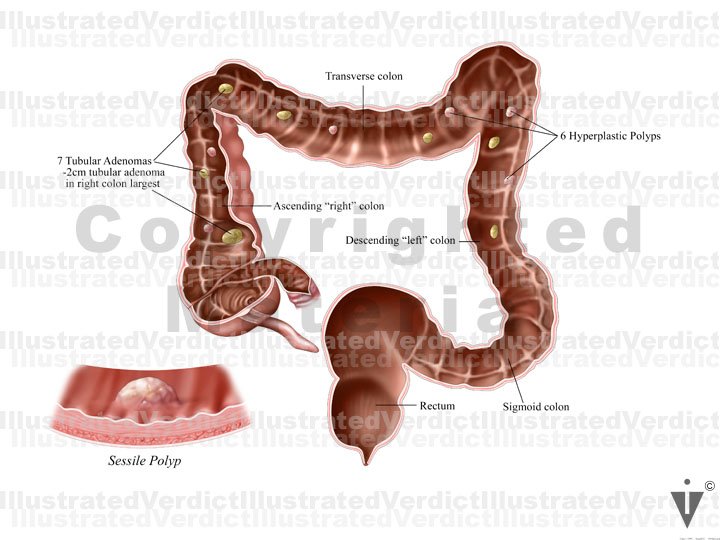
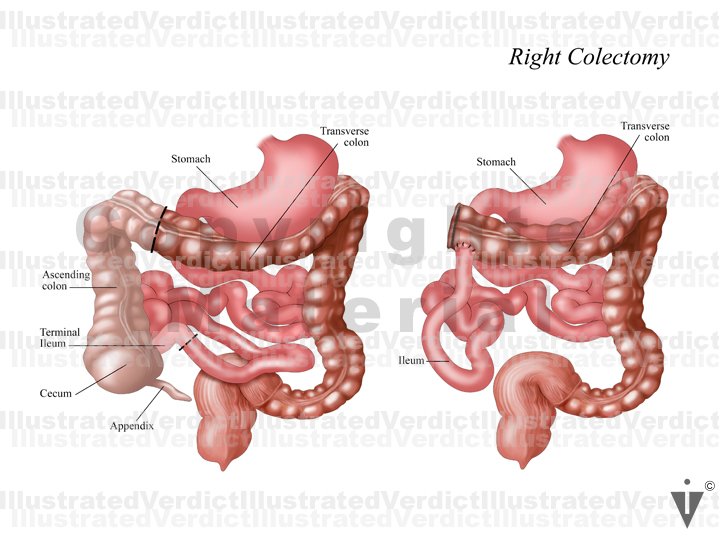
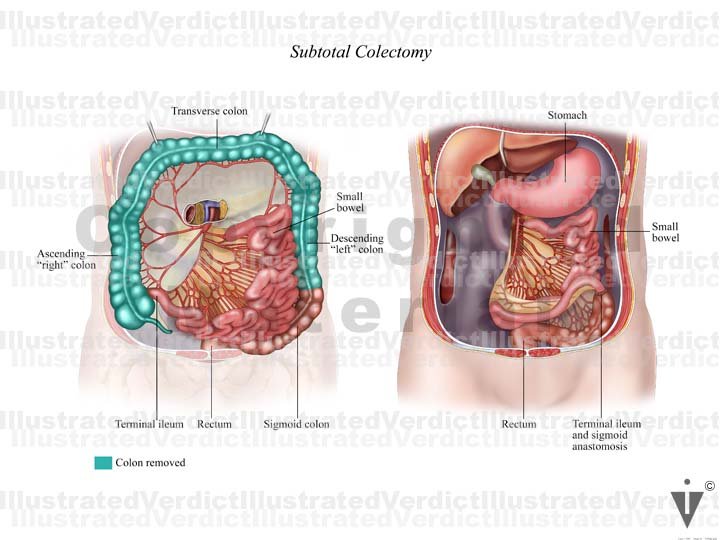
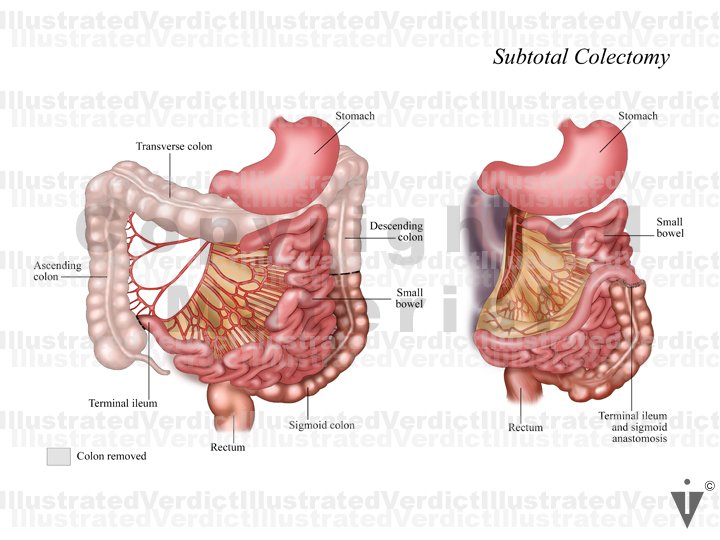
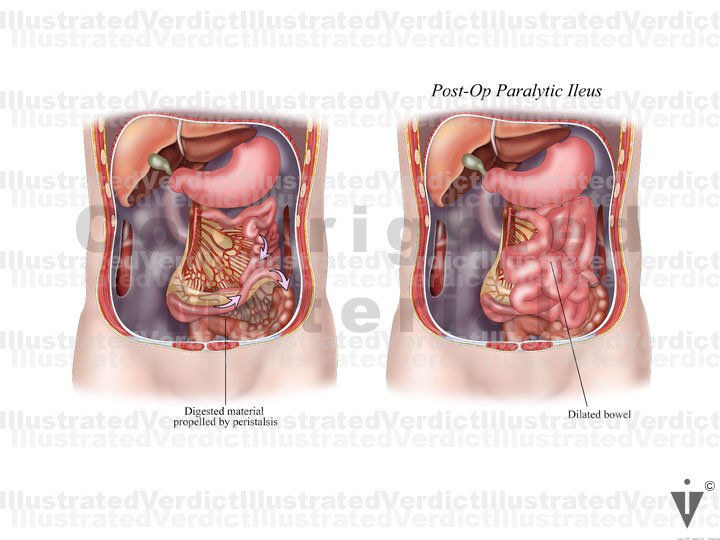
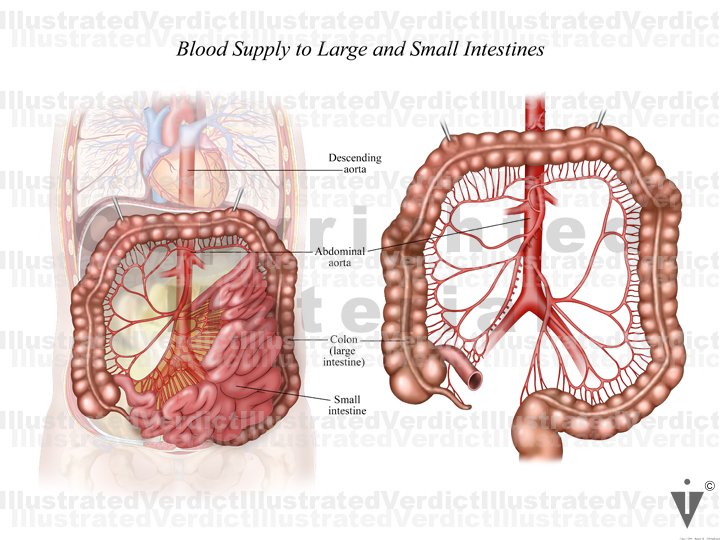
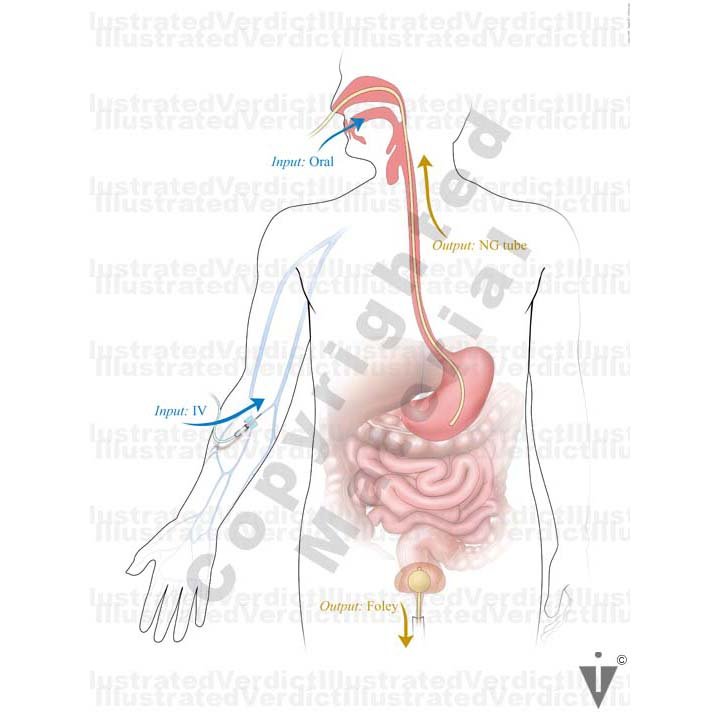
Pathology showed seven tubular adenomata and six hyperplastic polyps. Patient agreed to subtotal colectomy. He did well during his hospitalization and he was discharged. Three days post op he reported having 24 hours of abdominal pain, nausea and vomiting, he was instructed to come to ER immediately. He had an abdominal/pelvic CT scan that showed multiple loops of dilated small bowel. Postoperative ileus or small bowel obstruction were considered. The plan was to try a conservative approach to give his bowel a rest with IV fluids, NPO (nothing by mouth) and NG tube suction. He began to decompensate the following day, with blood pressures and O2 sat falling. He was moved to the ICU and intubated. He was noted to have become septic with hypotension (low blood pressure), acidosis and acute renal insufficiency. Broad spectrum antibiotics were started, but he continued to decompensate. He was brought in for an exploratory laparotomy to look for a leak or ischemic bowel because he was not responding to the other therapies. A long segment of the jejunum was slightly blue but appeared viable. Unfortunately there was nothing to be done that could help his situation and they closed him up. He passed away a few days later. The autopsy showed that the descending and abdominal aorta had severe atherosclerosis with stenosis. The defense experts believed this played a role in his healing post op the first procedure and he was unable to recover. The jury found in favor of the defense.